The Wholesome Journey - Group Nutrition Coaching Program
Mentorship Program, 1:1 Nutrition Coaching with Alison
What do you want to learn more about?
Program Login
Podcast Features
January 27, 2026
Alison Tierney, MS, RD, CD, CSO
Alison is a registered dietitian, board-certified in oncology nutrition, and a cancer thriver. Her expertise in oncology nutrition and personal experience with her own cancer diagnosis and its treatment provide her with the unique perspective of being able to relate to her clients on an entirely different level. Her content is consistently focused on evidence-based guidelines and seeks to increase the awareness of the power of nutrition to complement traditional cancer therapies.
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
- Alison Tierney, MS, RD, CD, CSO
If you’re searching for DIEP flap before and after experiences, you’re likely looking for more than just photos. You likely also want to understand what recovery actually looks and feels like. In this post, I share my personal experience with bilateral mastectomy and immediate DIEP flap reconstruction. The post includes what I wish I had known before surgery, what the early days of recovery were really like, and how healing unfolded over time.
From hospital care and pain management to at-home preparation, this article offers an honest, patient-centered perspective. It covers movement, clothing, and long-term recovery in a way most resources overlook. And rather than focusing on surgical details, it centers on the real experience of healing. This article goes beyond the before-and-after photos found on surgeon websites. Instead, it shares the lived “before and after” of the DIEP flap journey.

What is DIEP Flap Surgery?
DIEP (or, deep inferior epigastric perforator) flap surgery is a type of breast reconstruction that uses a woman’s own tissue to recreate one or both breasts after a single or double mastectomy, respectfully.
The surgery involves a plastic surgeon transferring skin, fat, blood vessels, and sometimes nerves from the lower abdomen to the chest by then connecting the blood vessels in the chest using microsurgery. This part of the surgery ensures the reconstructed breast has its own blood supply.
Surgeons typically perform this procedure after a woman receives a breast cancer diagnosis. They may also perform it after a prophylactic mastectomy to help reduce risk in high-risk individuals. I had surgery before starting any additional treatment, which doctors refer to as adjuvant therapy.
A woman might choose DIEP flap breast reconstruction over breast implants for several reasons of her own. And I stand strong in that they are very much are her own reasons.
For me personally, I liked the idea that the tissue used in the reconstruction was entirely my own. Additionally, with having a known rheumatoid abnormality and a twin sister with an autoimmune disease, I felt more comfortable avoiding implants related to a higher risk of rejection than the average woman.
When considering and deciding what type of breast reconstruction you’ll have, be sure to talk to your own surgeon regarding your individual risks related to either reconstruction route – flap reconstruction verses saline/silicone implants. Rates of surgical complications vary widely based on patient factors, implant type, and surgical technique.
From this point forward, this article is intended to share my lived experience with DIEP flap reconstruction. Additionally, I’ll review recovery-focused insights and practical support tools.
Related Post → Cold Capping During Chemotherapy: My Personal Experience & Tips
This article is not meant to serve as medical or surgical guidance. (Nor is any of the information found on this website; please review my website disclaimer here for more details). Nor will this article it cover detailed surgical risks, complications, candidacy, costs, or decision-making. All of the above should be discussed with your individual and qualified plastic surgeon.
Instead, this blog focuses on the personal, practical, and often overlooked aspects of recovery that many patients – including myself – wish they had known beforehand.
How to Prepare for DIEP Flap Surgery
When it came to preparing for surgery, I had what felt like an eternity to wait—about eight weeks from my breast cancer diagnosis to my surgery date. During that time, there was still uncertainty around whether I would have immediate reconstruction or need to pursue delayed reconstruction at a later date.
Immediate reconstruction meant that my mastectomy and DIEP flap reconstruction would happen during the same surgery. This surgery included both a breast surgeon and a plastic surgeon. However, the surgical plan depended on what surgeons found during the operation.
My care team informed me they would perform a sentinel lymph node biopsy during the mastectomy. If the biopsy showed cancer in the lymph nodes, surgeons would complete the mastectomy and postpone DIEP flap reconstruction. In that case, I would need radiation therapy before moving forward with reconstruction.
Of note – at this time I had had an MRI, a biopsy, and a mammogram guided biopsy. I had surgery first, then completed additional treatment later, known as adjuvant therapy. Many women may have neoadjuvant treatment (before surgery) with the intention to shrink the tumor(s) prior to surgery. This would be for the purposes of having the best possible outcome.

Going into surgery without knowing whether I would wake up reconstructed—or facing additional treatment and a delayed reconstruction—was emotionally heavy and stressful on top of the distress a cancer diagnosis, loss of my breasts, and surgery itself carried.
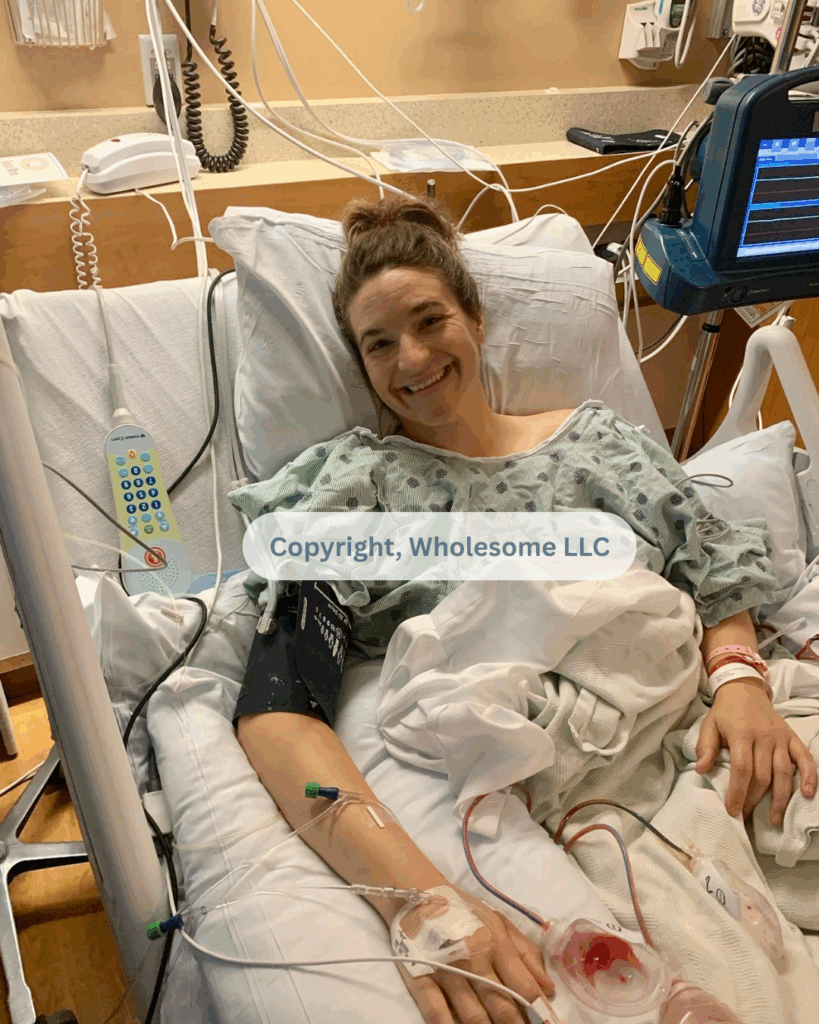
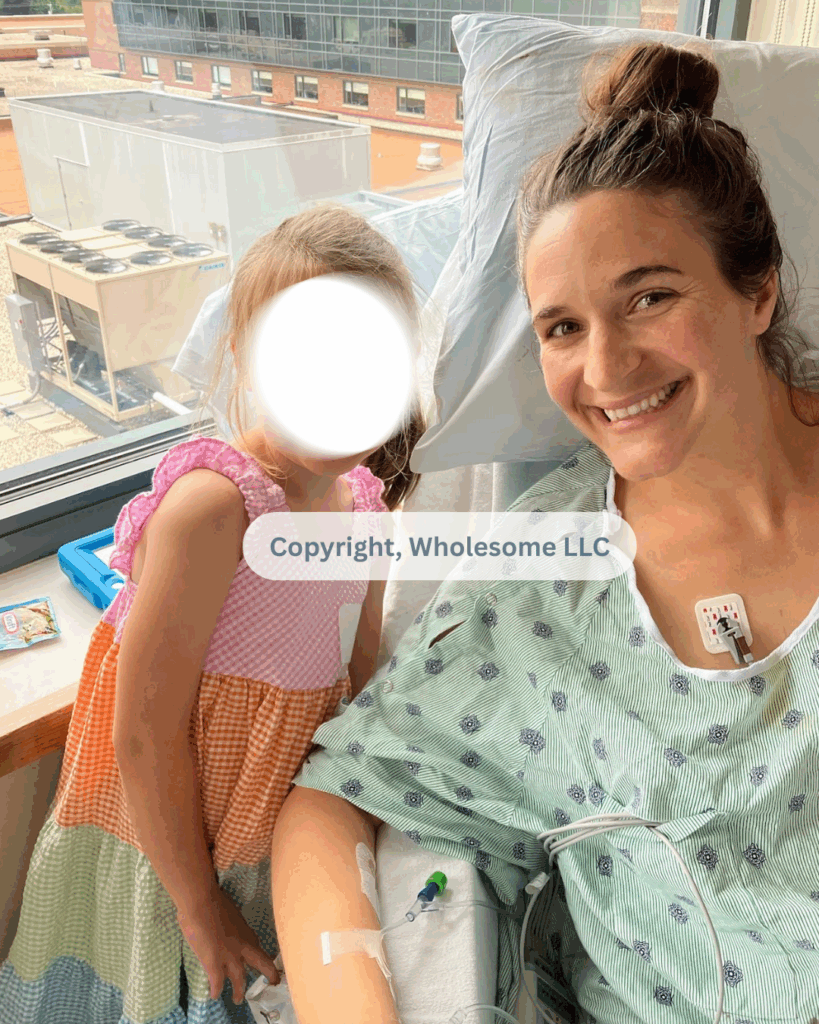
When I woke up after surgery and eventually had the energy to look down, I saw two newly reconstructed breasts. In that moment, I knew my sentinel lymph node was negative. The surgical team had been able to proceed with immediate DIEP flap reconstruction.
About a week later, however, surgical pathology revealed that I would still require chemotherapy and targeted therapy for triple-positive invasive ductal carcinoma. That news came as a surprise, since it differed from my diagnosis going into surgery. And yet, another reminder that even when one part of the plan moves forward, cancer care is rarely linear.
Home Prep: Setting Up for a Smooth Recovery after Bilateral DIEP Flap Reconstruction Surgery
I had my DIEP flap surgery in July of 2022. At the time, my oldest daughter was 5 years old, and my youngest daughter was 17-months old. Needless to say, it would take a village to help myself and my family get through surgery and recovery. Whether you have younger children or not, having support of family and/or friends is paramount. Not only should you have an understanding of what to expect, but also those that will help care for you.
Here are my top recommendations to get ready for surgery –
1. Ask for and accept help.
Like many women, before my cancer diagnosis I struggled to ask for and accept help. But the truth is, we aren’t meant to navigate life alone. At diagnosis, I made a quiet vow to myself: I would ask for help—and I would accept it.
So when someone offered to bring a meal, I said yes.
When someone offered to run errands or pick up groceries, I said yes.
When someone offered to help with childcare or host a playdate (of course, with people I trusted), I said yes.
Personal tip: A mindset shift that helped was remembering that helping often feels good for the helper, too. Yes, I needed support. But allowing help gave others a meaningful way to show up for me and my family.
I am deeply grateful for the strong support system I have. My parents live just 20 minutes away, which makes a significant difference. I know this level of support isn’t available to everyone. Still, I encourage you to identify at least one person for in-person support after surgery. Having physical help during recovery can make a meaningful difference.

✨ Click here for 50% off your first week, 20% off weeks 2–3, and 10% off weeks 4–5
2. Think Through Your Sleeping Setup
After surgery, I slept in a recliner for five and a half weeks. I didn’t feel comfortable transitioning back to my bed right away. I’m a side sleeper, which likely contributed to needing extra time. Lying on my side felt challenging with fresh mastectomy incisions.
I was incredibly fortunate my parents provided a power-lift electric recliner – similar to this one. It reclined nearly flat, assisted me to standing, and supported me while sitting. The lift feature was especially helpful with the large abdominal incision.
Several clients with DIEP flap reconstruction found adjustable beds extremely helpful. Head and foot elevation improved comfort, sleep quality, and early independence.
If a recliner or adjustable bed isn’t an option, consider a bed wedge pillow set. Wedge pillows support your upper body and legs during recovery. They reduce strain when getting in and out of bed. They also create a more comfortable sleeping position early on.
The Key Takeaway: plan your sleeping setup ahead of time, and adjust as needed once you’re home. Comfort, positioning, and ease of movement matter more than you might expect during recovery.
3. Establish a Recovery Nest
I’ll never forget pulling into our driveway after surgery and seeing the excitement on my little girls’ faces. As happy as I was to be home and reunited, I walked through the door and headed straight for my ‘recovery nest’—a space my husband and I had intentionally set up in our bedroom to support rest and healing.
I’ll never forget pulling into our driveway after surgery and seeing the excitement on my girls’ faces. Coming home and reuniting with them filled me with joy. Still, I headed straight to my “recovery nest.” My husband and I intentionally created this space to support rest and healing. We intentionally set it up in our bedroom to make rest and recovery easier.
At the time, we didn’t have a TV in our bedroom. My sister generously let us borrow one during my recovery. I wasn’t sure how much time I’d spend there initially. But, having a calm, comfortable space that felt like mine mattered deeply.
My recovery nest centered around the power-lift recliner. We kept other essentials close by or easy for myself or my husband to grab. One favorite addition was an adjustable side table. It didn’t feel overly “hospital-like,” which I appreciated. It held my water bottle, medications, books, and other essentials. Bonus: I later repurposed it as a standing desk in my home office!

If you’re setting up your own recovery nest, consider including:
- A comfortable recliner or supportive chair
- Blankets
- Water bottles – One filled with water; One filled with an electrolyte drink, such as ElectroMag™ by True Grace.
- Extra pillows or cushions for positioning and comfort
- An adjustable side table
- Medications
- Snacks
- Books and/or Kindle
- Phone charger
- Lotion
- TV remote
This doesn’t need to be elaborate or perfect—just intentional. Creating a space where everything you need is within reach can make those early recovery days feel far more manageable.
Pro Tip: Consider using an audio baby monitor or similar device during recovery. It allows you to easily call or speak to your caregiver from another room.
4. Consider Your Shower Setup
I spent three nights in the hospital. Once home, my surgeon gave me permission to shower and get my incisions wet. That said, always check with your own surgeon, as post-op showering guidelines can vary.
If I’m being completely honest, showering was one of the most difficult parts of my early recovery—especially during the first two weeks. Between the discomfort of multiple incisions and limited arm mobility, I wasn’t able to wash my hair or shower independently.
To make showering possible, I used a shower chair with a backrest, and my husband helped with did all of the washing. Physically, it was exhausting. Emotionally, it was humbling—there’s a certain grief that comes with losing independence, especially at 33, and needing your spouse to bathe you. We didn’t expect it, but it became part of the season we were navigating.
During those early weeks, showering felt like an athletic event. I could manage the shower itself, but afterward I immediately needed to return to my recovery nest to rest and recover.
To make bathing easier during recovery, consider the following:
- A shower chair with a back (and make sure it fits in your shower before surgery)
- Shower-friendly drain holders (I had six drains during the first week—plan for more than you think you’ll need)
- A handheld shower head
- Waterless shower cloths or wipes for days when a full shower feels like too much
- Dry shampoo (especially helpful early on)
There is no “right” way to do this—only what feels manageable and safe for you. Planning ahead can make an emotionally and physically challenging part of recovery feel just a little more doable.
A Gentle Reminder: Recovery from DIEP flap reconstruction and mastectomy is not linear. Everyone moves through healing at their own pace. Please don’t compare your timeline to mine. These milestones reflect my personal journey, not a standard to measure yourself against.
5. Consider Clothing
After a mastectomy and/or DIEP flap breast reconstruction, you’ll want to plan for different clothing needs—at least for a while. As with everything shared here, be sure to follow the specific post-op guidelines provided by your plastic and breast surgeons, especially when it comes to compression garments, as recommendations vary.
In my case, my plastic surgeon shared that he performs DIEP flap reconstruction a bit differently based on the blood vessels used. Because of that, I was NOT to wear post-surgical compression garments or bra over the reconstructed breasts for at least six weeks following surgery. Many surgeons recommend compression during this time, including breast and abdomen or thigh compression.
Be sure to ask your surgeon what they recommend specifically for you.
It’s also worth noting that during my two revision surgeries following my initial DIEP flap reconstruction, I did wear post-surgical compression garments. In those cases, the garments were provided by my surgical team. Be sure to ask your surgeon ahead of time whether you’ll need to purchase any garments yourself or if they’ll be supplied after surgery.
When I was finally cleared to wear a bra (around six weeks post-op), I transitioned into these bras (since they have no underwire) and have worn them exclusively since my surgery in July 2022.
For the early recovery period, I made sure I had the following clothing on hand:
- PJ tops with drain pockets (I recommend at least 2–3 so you always have a clean option). Honestly, I wore these to post-op appointments during the first couple of weeks—comfort mattered far more than how I looked.
- Loose, comfortable pajama pants, especially important given the large abdominal incision and in the earlier days of recovery
- Choose button-down shirts or zip-up sweaters to avoid pulling clothing over your head.
- Soft, stretchy bottoms for later recovery and when you don’t want to wear PJ pants (I wore maternity shorts I still had at home, which were surprisingly perfect over healing abdominal incisions)
- Slip-on shoes that don’t require bending or tying. This may sound like a small thing, but it made a big difference! I already owned Kiziks before surgery and was so grateful for them during recovery.
- Abdominal and/or thigh compression garments – Although I personally did not wear these after my initial DIEP flap surgery, my surgeons did have me wear compression during one of my revision surgeries (which also included a hysterectomy). Many surgeons require abdominal and/or thigh compression after DIEP flap reconstruction, so be sure to clarify ahead of time what will be recommended for you.
- Mastectomy pillow, more specifically used for car rides. There are many listed on Amazon, however, I had a homemade one that was borrowed to me from a friend.
Gentle Reminder: Comfort, accessibility, and ease of movement are the priorities here. This is not the season for “pushing through” or doing all the things —it’s the season for making things simpler wherever you can.

6. Other Helpful Tools in Recovery
Following surgery, there were a few tools I found surprisingly helpful during recovery—items I didn’t initially associate with surgery, but that ended up making a meaningful difference. I wanted to share them here in case they’re helpful for you, too.
Theragun (or similar massage device)
I had received a Theragun for Mother’s Day earlier that year—before my diagnosis—and originally used it for chronic back pain unrelated to cancer or surgery. During recovery, however, I was far less active than usual and spent much more time sitting. As a result, my back and even my tailbone became incredibly uncomfortable—at times, almost more so than my surgical incisions. The Theragun was a true saving grace. Interestingly, another friend who also had DIEP flap reconstruction shared a similar experience and found significant relief after trying it as well.
(Of course, I did not use the device on or near incisions, but instead on my back and buttocks for pain relief strategies I already knew from my lifelong battle with chronic back pain. If you are unsure, at a physical or occupational therapist how to use a similar device.)
Tailbone relief seat cushion
During my pregnancies, I struggled with tailbone pain, and my physical therapist had recommended a seat cushion designed to relieve pressure in that area. I found myself reaching for this cushion often during recovery, especially when resting in my recovery nest. It helped make extended periods of sitting much more tolerable.
Both of these items were things I already owned and weren’t purchased specifically for surgery—but they ended up being incredibly helpful in supporting comfort during recovery. Sometimes it’s the unexpected tools that make the biggest difference.
The Surgical Experience: What I Experienced & How it Felt
I’ll never forget the night before surgery or the drive to the hospital that morning of surgery. There were so many emotions swirling at once—anger, fear, sadness, grief, and, unexpectedly, gratitude. Gratitude for having a surgical option. And gratitude for an early-stage diagnosis.
Alongside all of that, there was a deep uncertainty about what recovery would actually feel like.
Before my surgery, I was incredibly grateful to a client’s daughter (we’ll call her Jane for the purpose of this article) who generously shared her own experience with me. She offered insights my surgeon hadn’t covered—not because they were unimportant, but because they were the lived, day-to-day realities I didn’t yet know to ask about. That conversation helped me feel more mentally and emotionally prepared going into surgery.
That experience is why I want to share more of mine here. While I won’t be diving into the technical details of the procedure itself—that’s a conversation best had with your surgeon—my goal is to pay it forward, just as someone did for me, by sharing what the surgical experience felt like and the things I wish I’d known beforehand.
Waking Up After My Bilateral Mastectomy with DIEP Flap Breast Reconstruction
I was told my surgery could take up to 10 hours, given that I was having both a bilateral mastectomy and DIEP flap reconstruction. The first thing I remember after waking up was an overwhelming sense of grogginess—drifting in and out of sleep, barely aware of time passing.
Once I had enough energy to open my eyes, I remember looking down and seeing two reconstructed breasts. In that moment, I felt deeply relieved—but also incredibly exhausted.
I had been informed ahead of time that two aspects of my post-operative care were standard protocol for my surgeon. First, I would spend the initial night in the ICU, where I could receive one-to-one nursing care. Second, I would have an epidural in place to help manage the abdominal pain.
Since then, I’ve learned that neither of these practices are universal for all DIEP flap procedures/surgeons, so it’s worth asking your surgeon what post-op monitoring and pain management will look like for you. While I can’t compare recovery with and without an epidural, I can say that I was very grateful to have one. I didn’t experience significant pain—more discomfort than anything—which made those first hours and days more manageable. However, Jane, who didn’t have an epidural for her DIEP Flap, shared she experienced the most pain she’d ever experienced in her life, following surgery. 🙁
One detail I hadn’t fully anticipated—but had been warned about by Jane—was how warm my hospital room would be kept after surgery. She was right. It was intentionally very warm, and it definitely added to my discomfort.
My surgeon later explained that the elevated room temperature helps support blood perfusion (blood flow) to the newly reconstructed breasts (the flaps). While medically necessary, it wasn’t comfortable.
Two small adjustments made a big difference for me:
- I asked my nurse to put my very long, thick hair into a bun on top of my head. It had been draped around my neck and was making the heat feel worse.
- She also brought me a small bedside fan, which helped tremendously.
I will forever be grateful for that nurse. Sometimes it’s the smallest comforts that make the biggest difference in those early hours and days.
As a side note, although my husband initially planned to stay overnight with me at the hospital, I encouraged him to go home and get some good sleep. He later told me he was incredibly grateful—especially given how warm the room was!
The following morning, after my plastic surgeon completed rounds and felt I was doing well, I was transferred to a regular surgical floor—complete with a normal room temperature. Thank God!
My Hospital Stay: Navigating the Early Days of Recovery
Going into surgery, I was told to expect a 3–5 night hospital stay. My plastic surgeon felt confident I would only need three nights, while the anesthesiologist—who managed my epidural during and after surgery—was less convinced and suggested that staying just three nights would be unlikely.
Thankfully, my surgery and hospital recovery were free of complications. That said, DIEP flap reconstruction is a complex procedure and does carry a higher risk of complications compared to some other reconstruction options. Because of this, it’s important to talk with your plastic surgeon about what potential complications could look like—both during surgery and in the days immediately following.
From there, the length of my hospital stay was largely determined by how well I tolerated pain as my epidural was gradually reduced. My anesthesiologist used an infusion scale from 0–10 (I believe measured in mL/hr). Immediately after surgery, my epidural was set at 10.
Overnight in the ICU, it was decreased to 8 due to minimal pain. From there, the plan was to slowly decrease the infusion by 2–3 points at a time, as long as my pain remained manageable.
Looking back at my hospital progress notes, here’s how that process unfolded:
Day of Surgery – Day 0
- Arrived in the ICU by 6:45 PM
- Epidural: 10
Post-Op, Day 1
- 4:06 AM: Epidural decreased to 8; bedrest
- 11:48 AM: Epidural decreased to 6; bedrest
- 1:35 PM: Pain 3/10 (self-reported 🙃)
- 8:35 PM: Epidural 6; pain 3/10
Day 2 Post-Op
- 4:00 PM: Epidural decreased to 3; pain 3/10
- Walked to (a few steps) and sat up in a chair for the first time 🎉
Day 3 Post-Op
- 9:52 AM: Epidural turned off
- Took one full walk around the hospital floor
- 4:00 PM: Discharged and home ❤️
Again, I share my progress here not as a comparison or expectation for what your journey should look like, but simply to offer a glimpse into my experience and help gently manage expectations. There is no “right” timeline—your body will heal at its own pace. Pain management is closely monitored and tailored to you as an individual. And while progress can feel like a series of very small steps, each one is meaningful.
Healing from a Bilateral Mastectomy with Immediate DIEP Flap Reconstruction
I’ve shared a bit of my healing journey at home within this blog above, where I outlined a lot of the things that helped me on my journey. Beyond this, I wanted to share a few more insights regarding my recovery.
What is the recovery timeline for DIEP Flap Reconstruction?
My surgeon shared with me to expect about a 12-week recovery. Since I worked (and still work) for myself, I was thankfully able to take the time away from work that I needed.
As noted earlier, I truly felt like the first 2 weeks were the most difficult between discomfort, showering, and actually taking care of myself. From there, I slowly started to feel more and more like myself, every day.
I didn’t spend as much time in my recovery nest as I expected upon my return home. I actually felt best being among the hustle and bustle of my family, even if it just meant sitting the in same room as them or moving from one chair to the other.
My family and I were blessed to have my in-laws stay with us for a few day post-op so my husband could focus on caring for me, while Grandma & Grandpa were able to care for my two, young daughters.
Gradually Increasing Physical Activity After Surgery
On day four post-op, I began taking short, daily walks outside. We’re incredibly fortunate to live in a safe neighborhood with sidewalks, and it was July in Wisconsin at the time—which made getting outside much easier.
(As I’m writing this now, we’re expecting a –12°F (–24°C) high tomorrow, with a –31°F (–34°C) low. 🥶 That kind of weather would have made early movement much more challenging post-op.)
At first, my walks were very short—literally to the end of the block and back, maybe 100 yards total—and always with my husband. Each day, I’d aim to go just one mailbox farther…then maybe repeat it later in the day. Small, intentional progress.
By my two-week post-op appointment with my breast surgeon, I was able to walk to the hospital. To be clear, the hospital is only 0.7 miles (1.1 km) from our house, I walked with my husband, and I had my dad “on-call” in case I couldn’t walk home—but I did. 🙃
My surgeon was shocked. She even joked, “Don’t tell anyone you did that—you’ll make this surgery look too easy!” (And yet… here I am, sharing it.)
I want to be very clear: this surgery and recovery are anything but easy. It has been the hardest thing I’ve ever gone through—physically, mentally, and emotionally.
That said, it’s my strong (and yes, somewhat biased—as a dietitian) belief that the foundation I had going into surgery—combined with supportive nutrition, lifestyle habits, and a focus on slow, steady movement afterward—played a meaningful role in my recovery.
(I’ll be sharing more about nutrition and lifestyle considerations before and after surgery in a separate post—stay tuned. In the meantime, check out my post: Health 101: Does Sugar Feed Cancer?)
Post-surgery, I had strict lifting restrictions, which meant I wasn’t picking up my baby or young daughter for quite some time. I noticed that on days I felt better, I naturally wanted to do more—but I also had to be very mindful. My body was quick to let me know when I’d overdone it: increased abdominal pain or swelling were clear signals to slow down.
While I was given a 12-week recovery timeline, full recovery to your “new normal” can take much longer. In my case, I began chemotherapy and targeted therapy at six weeks post-op, which understandably slowed healing even further.
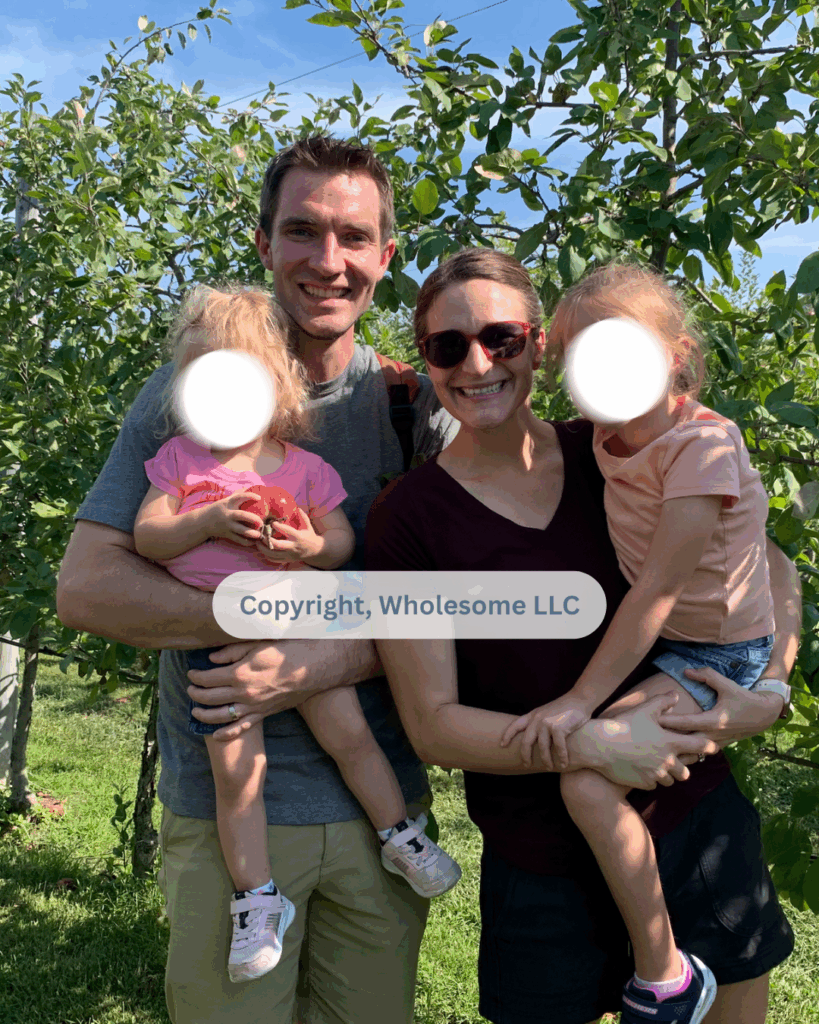
Still, I’ll never forget the first time I picked up my 5½-year-old daughter again. It was 9-weeks post-op, at a local apple orchard. A stranger offered to take a family photo, and without even thinking, I lifted her into my arms. Afterward, she looked at me and said, “Mama… you just picked me up for the first time in a very long time.”
My heart burst.
My Long-Term Recovery from Surgery
At the time of this writing, I am 3.5 years out from my double mastectomy with immediate DIEP flap reconstruction. Since that initial surgery, my body has been through a great deal: three months of chemotherapy, twelve months of targeted therapy, endocrine therapy (which I ultimately chose to stop after 1.5 years), one breast revision surgery, and a second breast revision surgery that was combined with a hysterectomy.
It’s safe to say that my body is not what it once was—but over time, I’ve found my new normal.
Are my breasts perfect? Absolutely not.
Is my core different? Yes—and I still notice some limitations with certain core-focused movements.
That said, the DIEP flap surgery itself does not prevent me from participating in exercise or movement. With time, support, and adaptation, I’ve learned what works best for my body now.
Looking back, I am confident in my decision to choose DIEP flap reconstruction. It was the right choice for me. If I were faced with the same decision again, I would make it again—without hesitation.
And while I feel at peace with my decision and have found my new normal, there are a few aspects of this surgery that surprised me—things I don’t regret, but wish I had understood more fully ahead of time. I want to share those here, not to deter, but to help you make the most informed decision possible.
What Was Unexpected for Me
Before I close out this post, I want to share a few things that caught me off guard—details I would want someone considering DIEP flap reconstruction to understand as they decide whether it’s the right choice for them.One of the biggest surprises was the degree of sensation loss. I have no sensation in my breasts, which I expected (but I can feel touch on my breast bone). What I didn’t fully anticipate was the extent of sensation loss in my abdomen. Roughly two-thirds of my abdomen, along with most of my mons pubis, lack sensation. Sensation below that area is intact, but the numbness itself was more significant than I had realized going into surgery. That said, the degree of sensation loss—or preservation—can vary widely depending on the surgeon, surgical technique, individual anatomy, and other factors.
It’s also worth noting that some surgeons now offer sensation-sparing mastectomies and reconstruction techniques aimed at preserving or restoring sensation to the breasts or nipples. These options weren’t part of my surgical plan, but if sensation is important to you, it’s absolutely worth discussing with your surgeon or a surgeon that is experienced in these techniques.
Another unexpected change has been reduced sensation along the backs of my upper arms—especially on the left side. It may sound minor, and for the most part it is, but it can be surprisingly frustrating. When I have an itch on my arms, breasts, or abdomen, it’s often difficult to fully relieve it because of the altered sensation!
None of these realities would change my decision—I would still make the same choice today. But they are details I wish I had better understood beforehand.

A Final Few Words
If you’ve made it this far, I want to start by saying thank you. Writing this post has been both reflective and emotional for me—and my hope is that reading it has helped you feel a little more informed, a little more prepared, and a little less alone.
DIEP flap reconstruction is a major surgery. The recovery is real, layered, and deeply personal. There is no single “right” experience, no perfect timeline, and no universal outcome. What matters most is that you feel supported, informed, and empowered to make the decisions that are right for your body, your values, and your life.
I share my story not as a blueprint—but as a lived example. One experience among many. If this post helps you ask better questions, set more realistic expectations, or feel more grounded as you move forward, then it has done exactly what I hoped it would.
I’d Love to Hear from You 💛
- If this post was helpful, I’d be grateful if you let me know in the comments.
- If you’ve had DIEP flap reconstruction yourself, I invite you to share anything you would add from your experience—your insights may be exactly what someone else needs to hear.
- And if you’re early in this journey and have questions, please feel free to ask them below and I’d be happy to answer them, if I can.
This space is meant to be one of honesty, compassion, and shared wisdom. We don’t get through this alone—and we’re not meant to.
With you in this! 💪

DIEP Flap Before and After: Recovery & What I Wish I’d Known
Featured Articles
Wholesome LLC is not a medical practice, and its employees cannot offer medical advice. This website provides educational information but it is not a substitute for medical advice from a licensed medical professional who is familiar with your particular facts and circumstances. The information contained on this website is not intended to diagnose, treat, or cure any disease and shall not be construed as medical advice. The information and education on this website is provided for you to use at your own discretion.
You can further review our disclaimer here.
Wholesome
About Alison
Courses & Programs
The Wholesome Journey
Free Resources
FAQs
Press & Media
Recipes
Blog
Contact Us
Shop
© 2026 Wholesome, LLC All rights reserved.
Privacy Policy
Terms of Use
Disclaimer
Mobile Terms of Service